In recovery systems, reassurance often comes from absence. No crisis reported. No re-referral triggered. No formal indicators breached. On paper, recovery appears to be holding. In practice, this apparent stability can conceal growing vulnerability.
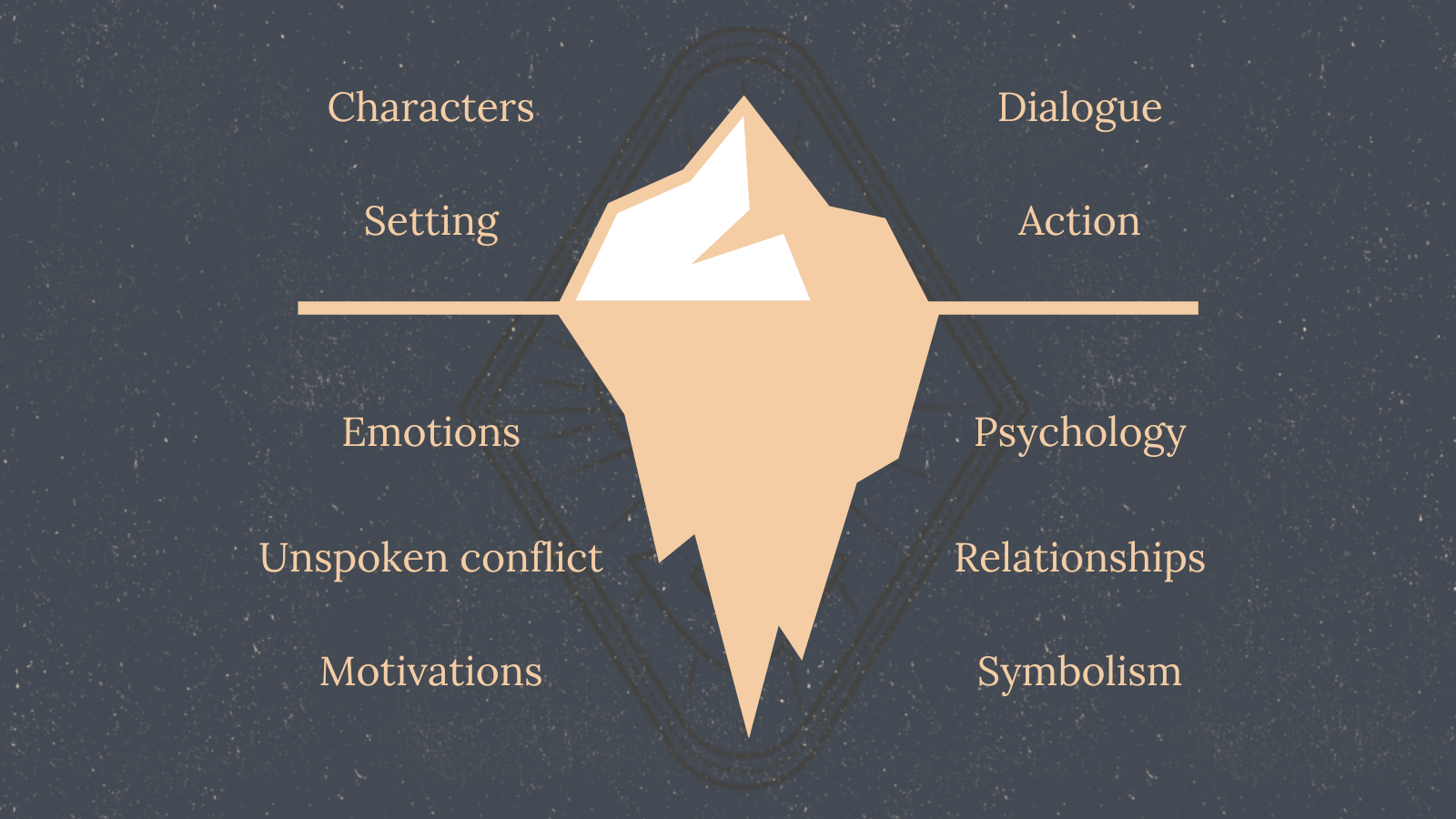
Recovery indicators play an important role in assessing progress. They signal whether immediate risk is present, thresholds are met, and formal pathways can close. What they do not capture is how recovery holds once those indicators fall quiet.
The Comfort of “Doing Okay”
Following discharge, many individuals present as “doing okay.” They attend appointments, report manageable symptoms, and appear to be functioning within expected parameters. These signals are often interpreted as evidence that recovery is consolidating.
Yet recovery is not a fixed state. It fluctuates in response to context, demand, and capacity. The appearance of coping can coexist with mounting strain, particularly when individuals are adjusting to new environments, reduced support, or cumulative stressors. What looks like stability may simply be the absence of immediate failure.
Why Vulnerability Is Easy to Miss
One of the defining challenges in long-term recovery is timing. Stressors rarely translate into immediate deterioration. Instead, their effects often emerge gradually, through fatigue, withdrawal, loss of confidence, or reduced engagement. These changes may not meet formal thresholds for concern, yet they signal increasing fragility.
This lag between stress and visible decline creates a blind spot. Systems that depend on episodic review or discharge-based metrics are poorly positioned to detect slow shifts. By the time deterioration becomes visible, opportunities for early stabilisation may already have passed.


The Limits of Snapshot Indicators
Discharge outcomes and periodic assessments provide useful snapshots, but snapshots are not trajectories. They capture how someone is presenting at a specific moment, not how recovery is unfolding over time. When snapshots are treated as proxies for stability, risk becomes something that is assumed away rather than actively monitored.
Insights reflected in the PATS continuity narrative consistently point to this gap: recovery often appears stable precisely because the indicators being used are not sensitive to gradual change. The absence of negative signals becomes falsely reassuring.
Beyond Reassurance Toward Awareness
Recognising these limits does not require additional intervention or intensified treatment. It requires a shift in how recovery is interpreted. Stability cannot be inferred solely from the absence of visible problems. It must be understood in relation to context, demand, and trajectory.
Evidence from real-world recovery patterns shows that vulnerability frequently persists beneath the surface, even when formal indicators suggest otherwise. Systems that acknowledge this reality are better equipped to respond proportionately, not reactively, when change begins.
Closing Reflection
When recovery looks fine on paper, it is tempting to assume it is holding in reality. Often, it is not. The challenge is not to abandon indicators, but to understand their limits, and to design recovery systems that remain attentive to what unfolds quietly, gradually, and out of view.
Discover more from Trauma Pain Support Ltd.
Subscribe to get the latest posts sent to your email.